
Removes potentially toxic byproducts of certain medications

Breaks down nutrients from food to produce energy when needed

Helps your body fight infection by removing bacteria from the blood

Produces and protects most of the substances that regulate blood clotting
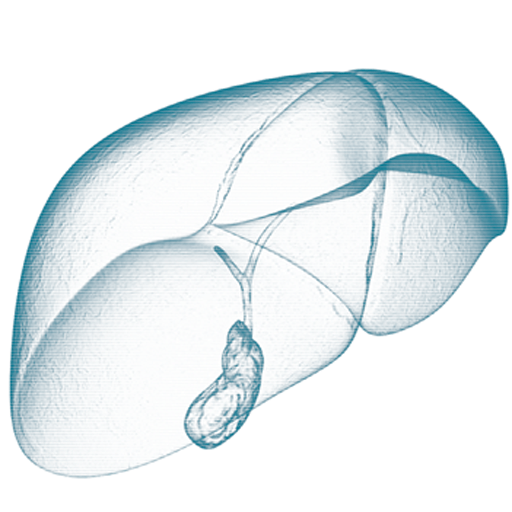

Prevents shortages of nutrients by storing vitamins, minerals and sugar

Produces most proteins needed by the body

Produces bile, a compound needed to digest fat and to absorb vitamins A, D, E and K

Bilirubin
Bilirubin is the main bile pigment in humans which causes the yellow discoloration of the skin and eyes called jaundice. Bilirubin is formed primarily from the breakdown of red blood cells. These breakdown products of the red blood cells are removed from the blood stream by the liver and secreted into the bile by the liver. Normally, the amount of bilirubin circulating in the blood is very low. However, conditions which cause increased formation of bilirubin, (such as destruction of red blood-cells), or conditions which reduce removal from the blood stream (such as liver disease) may result in an increase in the level of bilirubin in the blood. High levels of bilirubin cause jaundice.

Albumin
Albumin is a major protein which is produced by the liver. In chronic liver diseases, the amount of albumin produced becomes reduced as the disease progresses. Therefore, in advanced liver disease such as cirrhosis, the level of the albumin in the serum or bloodstream may be reduced.

GGT
Gamma Glutamyl Transpeptidase or GGT’s enzyme level is often elevated in liver disorders but can also be elevated in a wide range of other conditions such as diseases of the kidney, pancreas and prostate. However, when both the GGT and the alkaline phosphatase are elevated, doctors will look at liver causes first as the most likely explanation of the elevation.

AST and ALT
Alanine aminotransferase (ALT) and Aspartate aminotransferase (AST) are enzymes that are found in liver cells (hepatocytes) which help to process proteins. When the liver is injured or inflamed (such as in acute or chronic hepatitis), the level of ALT in the blood usually increases as the damaged liver cells leak the enzymes out into the bloodstream. ALT is more specific for liver disease than AST because AST can also be found in cell in the heart and muscle. The AST level in the bloodstream can therefore be high after a heart attack.

Alkaline Phosphatase
This enzyme level is increased in a large number of conditions that block or reduce the flow of bile out of the liver, such as gallstones or a mass or cancer blocking the bile duct. Other conditions such as injury to the bile ducts from a drug like an antibiotic or injury to the bile ducts cells following an alcohol binge (in alcoholic liver disease) may blocking the flow of bile in the smaller bile ducts within the liver. However, alkaline phosphatase is also found in other tissues such as bone. So doctors will also look at the GGT levels to be certain that the elevation in alkaline phosphatase is due to a liver problem.
We have become accustomed to hearing about the effects of unhealthy eating habits and being overweight on the heart. We know that many people are developing diabetes. Poor eating habits and being overweight can also harm the liver.
Fatty liver or Non-Alcoholic Fatty Liver Disease (NAFLD) is a term used to describe a condition caused by the build-up of fat in liver cells. A liver normally contains a certain amount of fat, but if fat represents more than 5% of the weight of the liver, that person is said to have “fatty liver” or steatosis. Fatty liver is a common condition that affects up to 17%-46% of European adult populations. It is the most common cause of chronic liver disease in developed countries. It is considered to be the hepatic manifestation of the metabolic syndrome. NAFLD presents as two distinct forms: simple steatosis (fat), and steatohepatitis or NASH, where fat in the liver causes inflammation. NASH is a more aggressive form of the condition, and some patients with NASH develop fibrosis, where the persistent inflammation in the liver results in the generation of fibrous scar tissue around the liver cells.
Fatty liver is usually associated with the following:
- Obesity, especially around the abdomen
- High cholesterol
- Type 2 diabetes
- High blood pressure
However, new research is suggesting a genetic involvement in the development of fatty liver. Some patients may be more genetically susceptible to developing fatty liver.
Fatty liver disease rarely causes symptoms until the liver disease is advanced. Fatty liver usually is found or suspected when:
- Abnormal liver tests are found on routine blood testing
- Fat is seen on ultrasound examination of the abdomen, performed for other reasons such as the diagnosis of gallstones
- The liver is enlarged on physical examination of a patient
The difference between isolated simple fatty liver and steatohepatitis (NASH) is the presence of inflammation and damage to the liver cells in NASH. Although about a third of the general population has fatty liver, approximately 10% have NASH. It is believed that the inflammation and damage of liver cells are caused by the toxic effects of the fatty acids released by fat cells.The consequences of fat in the liver depend greatly on the presence or absence of inflammation and damage in the liver, meaning, whether there is fat alone or NASH is present. Isolated fatty liver does not progress to significant liver disease. However, NASH can progress through the formation of scarring (fibrous tissue) to cirrhosis. The complications of cirrhosis include gastrointestinal bleeding, confusion (encephalopathy), liver failure, and liver cancer.
The main focus of treatment is lifestyle intervention including diet and exercise. It does not take large amounts of weight loss to result in a decrease in liver fat. Scientific studies have shown that a 10% decrease in body weight results in a significant reduction in liver fat-related inflammation and fibrosis in NASH patients. Scientific evidence suggests that the anti-oxidant Vitamin E may also help, reduce liver fat and inflammation and possibly fibrosis, but its long-term effectiveness and safety have not been well studied. New drug treatments are in clinical trials at the present time. In severe cases where liver failure has developed, liver transplantation may be required
Cardiovascular disease, especially heart attacks and strokes, is commonly seen in patients with fatty liver, and cardiovascular causes of death occur more frequently than liver-related deaths. Since the treatments for fatty liver disease are limited, it is important that the manifestations of the metabolic syndrome -obesity, high blood pressure, diabetes, dyslipidemia (abnormalities of lipids in the blood) – are aggressively treated.



Hepatitis C, or HCV, is a virus that infects and damages the liver. It can cause inflammation (swelling) and fibrosis (scarring) of the liver, which in some people can progress to cause serious liver damage such as cirrhosis. Co-infection means being infected with more than one virus. Some people with HCV infection may also be infected with HIV or hepatitis B virus.
For the majority of HCV-infected persons, the symptoms are non-specific and may include chronic fatigue, joint and muscle aches and pains, headaches, flu-like symptoms, discomfort in the liver area, depression, and poor concentration. But many infected persons have no symptoms.
The virus may cause:
- Dryness of the mouth and eyes
- Itchy skin
- Inflammation of the kidneys (glomerulonephritis)
- Thyroid gland dysfunction
- Insulin resistance and diabetes
- Increased risk of some types of cancer, such as non-Hodgkin’s lymphoma
HCV is curable for many people. Current treatment options can lead to a cure for the majority of patients with HCV. Treatment can clear the HCV virus from the body, meaning that the person is no longer infected and can no longer infect other people. Clearing the virus from the body improves liver wellness.
Until late 2014, the treatment options in Ireland for HCV meant taking a combination of an injection (Interferon) with tablets (Ribavirin). In 2015 new more successful treatments for HCV became available and are now the mainstay of therapy. These new drugs are called Directly Acting Antivirals (DAAs) and offer a cure for Hepatitis C in the majority of patients without advanced liver disease. DAA drugs work by blocking specific parts of the HCV virus directly, inhibiting or preventing many viral proteins from being produced by the HCV virus. DAA drug regimens usually consist of two or three drugs in combination, sometimes in a single pill, once or twice a day, all-oral (no injections) for 12 weeks. For some patients without advanced liver disease who have never had drug treatment in the past (treatment-naive), 8 weeks of DAA therapy is sufficient. Published data from clinical trials report that more than 90% of patients prescribed DAA therapies will successfully clear eradicate) the HCV virus. 12 weeks after completion of DAA therapy, a blood test (SVR12) is taken to assess for “sustained virologic response” or cure.
Hepatitis B is a serious liver infection caused by the hepatitis B virus (HBV). For some people, hepatitis B infection becomes chronic, meaning it lasts more than six months. Having chronic hepatitis B increases your risk of developing liver failure, liver cancer or cirrhosis — a condition that causes permanent scarring of the liver.
Most people infected with hepatitis B as adults recover fully, even if their signs and symptoms are severe. Infants and children are more likely to develop a chronic hepatitis B infection. A vaccine can prevent hepatitis B. If you are infected, taking certain precautions can help prevent spreading HBV to others.
Signs and symptoms of hepatitis B, ranging from mild to severe, usually appear about one to four months after acute HBV infection. Signs and symptoms of acute hepatitis B may include:
- Abdominal pain
- Dark urine
- Fever
- Joint pain
- Loss of appetite
- Nausea and vomiting
- Weakness and fatigue
- Yellowing of the skin and whites of the eyes (jaundice)
Sexual contact
Infection can occur through unprotected sex with an infected partner whose blood, saliva, semen or vaginal secretions enter your body.
Sharing needles
HBV is transmitted through needles and syringes contaminated with infected blood. Sharing drug paraphernalia puts you at high risk of hepatitis B.
Accidental needle sticks
Hepatitis B is a concern for health care workers who come in contact with infected human blood.
Mother to child
Pregnant women infected with HBV can pass the virus to their babies during childbirth. However, the newborn can be vaccinated to avoid prevent chronic infection.
If you suspect you may have hepatitis B, you should attend your doctor for an examination and blood tests. Blood tests can determine if you have the virus in your system and whether it is acute or chronic. Further blood tests can tell how much virus (HBV viral load) is in your body. A FibroScan® can assess how much damage (fibrosis) the virus has caused to your liver. Sometimes a liver biopsy may also be necessary.
Hereditary Haemochromatosis (HH) is a genetic condition of iron overload, which may result in excess iron stored in the liver, heart, joints and pancreas. Too much iron can lead to serious conditions such as liver cirrhosis, heart problems and diabetes. The genes that cause haemochromatosis (HFE mutations) are inherited, but the majority of people who have the genes never
develop serious problems, particularly if the diagnosis is made early in the course of the disease.
The HFE gene has two common mutations, C282Y and H63D. Genetic testing can reveal whether you have these mutations in your HFE gene. If you inherit 2 abnormal genes, you may develop haemochromatosis. You can also pass the mutation on to your children. Not everyone who inherits two genes develops problems linked to the iron overload of haemochromatosis. If you inherit 1 abnormal gene, you will not develop haemochromatosis. You are considered a gene mutation carrier and can pass the mutation on to your children.
While HH is present at birth, most people don’t experience signs and symptoms until later in life — typically between the ages of 40 and 60. Women are more likely to develop symptoms after menopause, when they no longer lose iron with menstruation and pregnancy. Common symptoms include joint pain, fatigue, and weakness.
Treatment includes regularly removing blood from your body. This is called venesection or phlebotomy. Because much of the body’s iron is contained in red blood cells, this treatment lowers iron levels. The amount of blood removed and how often it’s removed depend on your age, your overall health and the severity of iron overload. It may take a year or longer to reduce the iron in your body to normal levels. For further information on HH, see www.haemochromatosis-ir.com

